Human metapneumovirus (HMPV) is a leading respiratory virus that causes a wide range of respiratory illnesses, particularly in young children, the elderly, and immunocompromised individuals. It is responsible for a significant proportion of acute respiratory tract infections (ARTIs), often resulting in conditions such as bronchiolitis, pneumonia, and upper respiratory tract infections. These infections can lead to severe complications and, in some cases, contribute to substantial morbidity and mortality worldwide.
The virus, which belongs to the Pneumoviridae family, shares many clinical features with other respiratory viruses, such as respiratory syncytial virus (RSV), making it sometimes difficult to distinguish without advanced diagnostic methods. HMPV infections are typically seasonal, with outbreaks occurring more frequently during the winter and early spring months. Transmission of the virus occurs via respiratory droplets, and it is highly contagious, which further exacerbates its spread in households, healthcare settings, and crowded environments.

Despite the significant health burden posed by HMPV, there are no specific antiviral therapies currently available to treat infected individuals. The management of HMPV-related infections primarily focuses on supportive care, including oxygen therapy, hydration, and in some severe cases, mechanical ventilation. However, these measures do not address the underlying viral cause and often result in prolonged hospital stays and increased healthcare costs.
Furthermore, there is no licensed vaccine available to prevent HMPV infections, leaving vulnerable populations at high risk for severe outcomes. The lack of targeted treatment options and preventive measures underscores the urgent need for continued research into the development of effective antiviral drugs and vaccines. Scientists are actively investigating potential therapies, including monoclonal antibodies and antiviral agents, to fill this critical gap in healthcare.
In summary, human metapneumovirus represents a major public health concern, particularly for high-risk groups. The absence of specific antiviral treatments and preventive vaccines, combined with its seasonal and highly contagious nature, highlights the pressing need for more robust research and the development of effective therapeutic and preventive strategies to combat HMPV and reduce its associated burden on global health systems.
Acute respiratory tract infections (ARTIs) significantly contribute to global morbidity and mortality, posing a major threat to public health. These infections often progress to lower respiratory tract infections (LRTIs), responsible for millions of deaths annually. Viruses such as coronaviruses, influenza viruses, and human respiratory syncytial virus (hRSV) are common causes of ARTIs. In 2001, a novel virus linked to ARTIs, human metapneumovirus (HMPV), was discovered in the Netherlands. Since then, HMPV has been recognized as a leading cause of ARTIs worldwide, exacerbated by limited preventive and therapeutic options.
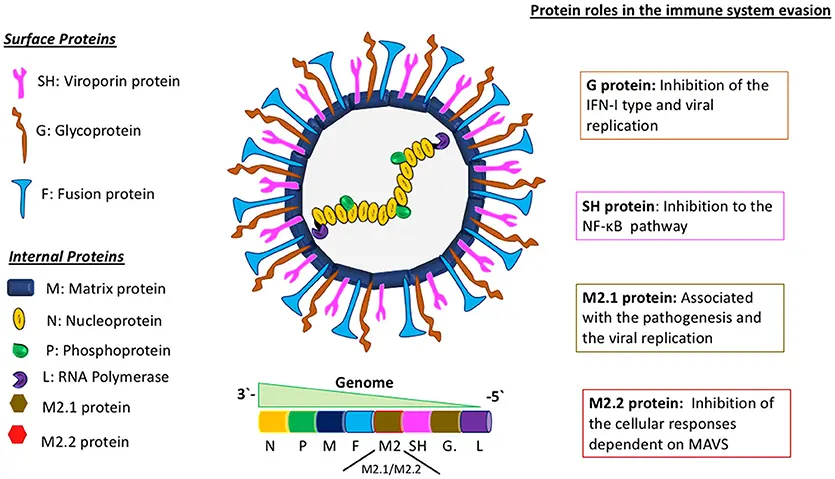
HMPV primarily affects infants, the elderly, and immunocompromised individuals, presenting symptoms like fever, cough, and difficulty breathing, similar to infections caused by hRSV and human bocavirus. This enveloped, non-segmented, negative-stranded virus belongs to the Pneumovirinae subfamily. Its genome (~13 kb) encodes nine proteins, including nucleoprotein (N), phosphoprotein (P), matrix protein (M), fusion protein (F), and glycoprotein (G). HMPV strains are classified into four genotypes (A1, A2, B1, B2) and six lineages (A1, A2a, A2b, A2c, B1, B2) based on the F and G genes. Co-prevalence of multiple sub-genotypes is common, though the relationship between genotype and disease severity remains unclear.
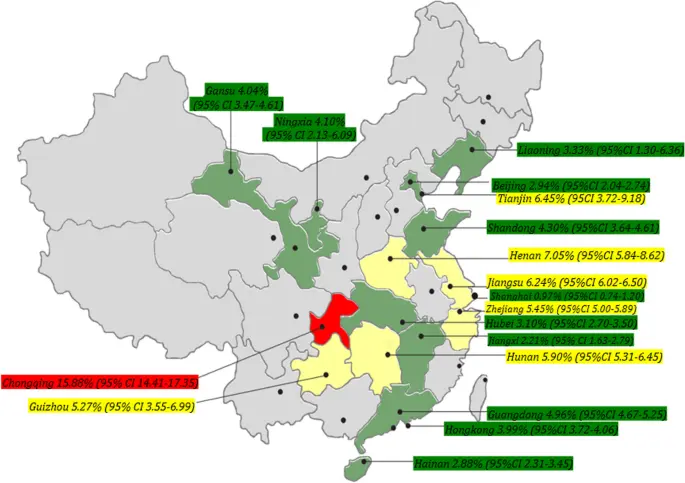
In China, HMPV was first identified in clinical samples during the early 2000s. Subsequent epidemiological studies revealed its significant contribution to ARTIs, particularly among young children, with outbreaks reported in multiple regions. Research has shown that HMPV infections are most prevalent during the winter and spring seasons, aligning with patterns observed globally. Studies have also highlighted the co-circulation of multiple HMPV genotypes in China, with certain genotypes more dominant in specific regions or seasons. The lack of effective vaccines and antiviral therapies has posed challenges, leading to a continued high disease burden, particularly among pediatric and high-risk populations.
HMPV infection imposes a significant medical burden, especially on children under five, accounting for nearly one million outpatient visits annually. The absence of licensed vaccines or antiviral treatments underscores the importance of understanding HMPV’s epidemiology, detection methods, and genotypic characteristics. This review highlights recent findings on HMPV in China, emphasizing diagnosis, prevalence, and genotype distribution.
Molecular detection methods based on PCR have advanced significantly for viral detection, including HMPV:

RT-PCR:
RT-PCR assays have been commonly used for detecting HMPV by targeting highly conserved genomic regions like the F and N genes, which are also used for genotype analysis. For example, Li et al. developed a GenomeLab Gene Expression Profiler (GeXP) multiplex RT-PCR method for detecting 16 ARTIs-related pathogens, including HMPV, with a detection limit of 1000 copies/reaction for each virus. However, due to its lower sensitivity and need for complex instruments, RT-PCR is now less utilized in clinical HMPV detection compared to RT-qPCR.
RT-qPCR:
RT-qPCR offers higher sensitivity, accuracy, and efficiency, making it the gold standard for viral nucleic acid detection. For instance, a TaqMan-based RT-qPCR method by Lu et al. detected HMPV at 10 copies/µL and identified more positive cases compared to RT-PCR. Sugimoto et al. developed a duplex RT-qPCR assay capable of differentiating HMPV A and B subgroups with a sensitivity of <10 copies/reaction. Additionally, multiplex RT-qPCR assays have been designed to simultaneously detect HMPV and other pathogens. For example, You et al. created a triple TaqMan-based RT-qPCR method for HMPV, RSV, and GAPDH detection with a sensitivity of 100 copies/reaction, while Feng et al. established a nested RT-qPCR assay to differentiate RSV, HRV, and HMPV with a sensitivity of 5 copies/reaction.
Recent innovations include combining RT-qPCR with digital microfluidic (DMF) technology for pathogen diagnosis. Huang et al. developed a platform for detecting 11 respiratory pathogens, including HMPV, with sensitivities of ≤150 copies/reaction off-chip and ≤120 copies/reaction on-chip.
Is Another Covid-like Pandemic Likely?

Experts believe fears of a Covid-style pandemic are largely exaggerated, explaining that such pandemics are typically driven by entirely new viruses, which is not the case with human metapneumovirus (HMPV). HMPV is already widespread globally and has been circulating for decades, meaning populations around the world have some level of existing immunity due to previous exposures.
According to Dr. Hsu, "Almost every child will have at least one HMPV infection by the age of five, and multiple reinfections are expected throughout their life." Paul Hunter, a medical professor at the University of East Anglia, added, "I don't think there are any current signs of a more serious global issue."
Despite this, health officials still recommend taking precautions to reduce the risk of contracting HMPV and other respiratory illnesses. These measures include:
• Wearing masks in crowded settings
• Avoiding crowds, particularly for those at higher risk of severe illness
• Practicing regular hand hygiene
• Disposing of tissues properly
Additionally, individuals may consider getting vaccinated against other respiratory illnesses like the flu. In the UK, pregnant women and adults aged 75 to 79 are encouraged to receive the respiratory syncytial virus (RSV) vaccine. RSV, while common and typically causing mild symptoms like coughs and colds, can lead to more severe complications in infants and older adults.
Learn more about Humain MetaPneumoVirus epidemiology and symptomes: